
By Jeannie Finnegan, CDP, Elder Care & Dementia Care Consultant
Mental health is important at every stage of life, from childhood and adolescence through adulthood, and yet mental health in later life is often sidelined as other health challenges are prioritized. However, there is a cyclical relationship between physical health and mental health: The presence of chronic conditions and illness is associated with an increased risk for mental illness, and we know that mental illness, in turn, increases the risk for many types of physical health problems.
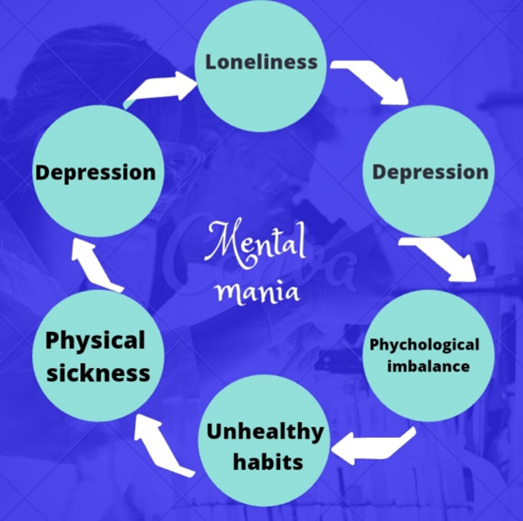
“Understanding Mental Health: Interrelation Between Loneliness and Depression”
Image credit: Hasibul Islam Apon. June 23, 2020
In addition, prolonged stress (such as the stress associated with the loss of a spouse or dealing with a chronic or serious illness) can cause depression by suppressing a person’s healthy coping skills, inducing persistent hyperactivity of the stress hormone system, even affecting the production and connection of nerve cells in the brain (The Journal of Neuropsychiatry and Clinical Neurosciences; Nov. 9, 2015). These changes can result in lowered mood, impaired concentration, irritability, and increased vulnerability to stress.
While anyone can experience depression, older adults may be more vulnerable. Older adults are more likely to experience multiple health challenges, isolation, and multiple major life losses. We also know that older adults with mental health disorders underutilize mental health services more than other adults, often afraid of the stigma historically associated with mental illness. More than 1 in 5 adults in the U.S. live with a mental illness.
However, a national survey by the GeneSight Mental Health Monitor conducted during the Covid-19 pandemic found that “nearly two-thirds of Americans aged 65 or older who are experiencing depression won’t seek treatment,” citing such reasons as the belief that their depression is “normal” and believing they should be able to handle it alone. About a third of seniors who think they are depressed believe that they can or should “snap out of it.” Other known barriers to help-seeking by older adults include difficulties with transportation, concerns about cost, fear of medication, and the belief that therapy is not likely to be effective.
“These individuals were raised in a time when anything that was considered a mental health problem was a personal shame and was to be denied at all costs,” says psychologist Patricia Farrell, Ph.D. “They saw mental health treatment as something that was for persons who were weak, unable to care for themselves, and inferior in some ways.”
This kind of thinking around mental health issues is a major obstacle to helping older adults overcome depression.
Symptoms of Depression in Older Adults
An important part of mental health awareness among older adults is recognizing the symptoms, which can be different from the symptoms of depression in other age groups. For many older adults, sadness is not the main symptom of depression. The National Institute on Aging lists some common symptoms in older adults as:
- Fatigue
- Trouble sleeping
- Irritability
- Confusion
While depression may present differently in older adults, it can also include other common symptoms of depression, including physical ones:
- Persistent sadness, anxiety, or “empty” mood
- Feelings of guilt or worthlessness
- Loss of interest in activities you once found pleasurable
- Appetite changes and/or unintended weight changes
- Difficulty concentrating
- Sleeping too much
- Aches and pains, headaches
- Thoughts of suicide
According to Deborah Heiser, Ph.D., an applied developmental psychologist specializing in midlife and beyond, “We have to look at older adults without the expectation that they should be depressed or that they should have physical infirmities — that backaches or headaches are normal,” Heiser says. “They’re not.”
We also know that mental health can change over time, depending on several factors. When the burdens a person experiences exceed their resources and coping abilities, it can greatly impact their mental health. For example, caring for a relative, experiencing chronic or life-limiting illness, extended social isolation, or experiencing economic hardship can all contribute to a decline in mental health. And while grief and bereavement are not the same as depression, they can be precipitating factors.
Unfortunately, because many older adults do not seek treatment for mental illness, alcohol is commonly overused and misused as self-medication by adults to cope with difficult life changes and resulting mental health challenges. Alcohol abuse among older adults is highly under-reported and overlooked. Rather than helping with mental illness, alcohol often has the opposite effect — it can contribute to depression, anxiety, withdrawal, and a host of other problems, such as memory loss, impaired balance, unstable diabetes, high blood pressure, gastrointestinal issues, adverse drug interactions, behavioral changes, and neglect of personal care.
How To Help Yourself or a Loved One
At any time in life, we can struggle with low self-esteem, feelings of sadness, hopelessness, loneliness, anxiety, anger, etc. There are times when getting support to boost mental health is a good decision. If you or someone you love have been experiencing several symptoms of depression for more than two weeks, or having suicidal thoughts, it is important to seek help. Depression is treatable! So, what are the best steps older adults should take to get the help they need?
- Talk about symptoms with a healthcare provider. This is important for ruling out medical or physical conditions before a mental health diagnosis can be made.
- Consider talk therapy with a counselor or licensed therapist. If transportation is a problem, telehealth is often a viable alternative to in-person therapy. Talk therapy can be used to explore feelings and thoughts, develop positive coping strategies, work on relationships, and make a plan for increased well-being.
- Joining a support group can help reduce feelings of isolation and provides a safe forum for sharing and discussions with peers around common challenges.
- Some primary care providers can help with common mental disorders, such as depression and anxiety. They might make recommendations for exercise and diet changes that can promote mental wellness.
- Your state’s Department of Aging may be able to refer to mental health resources in your community.
What to Do Next
If you are an older adult struggling with a mental health challenge or are concerned about a loved one who may be exhibiting symptoms of mental illness, we can help. Please call us at (443) 812-1028 for a complimentary 15-minute phone consultation, or use our contact form here. You may email us at help@stantonagingsolutions.com. We are your partners in care.

Leave a Reply
You must be logged in to post a comment.